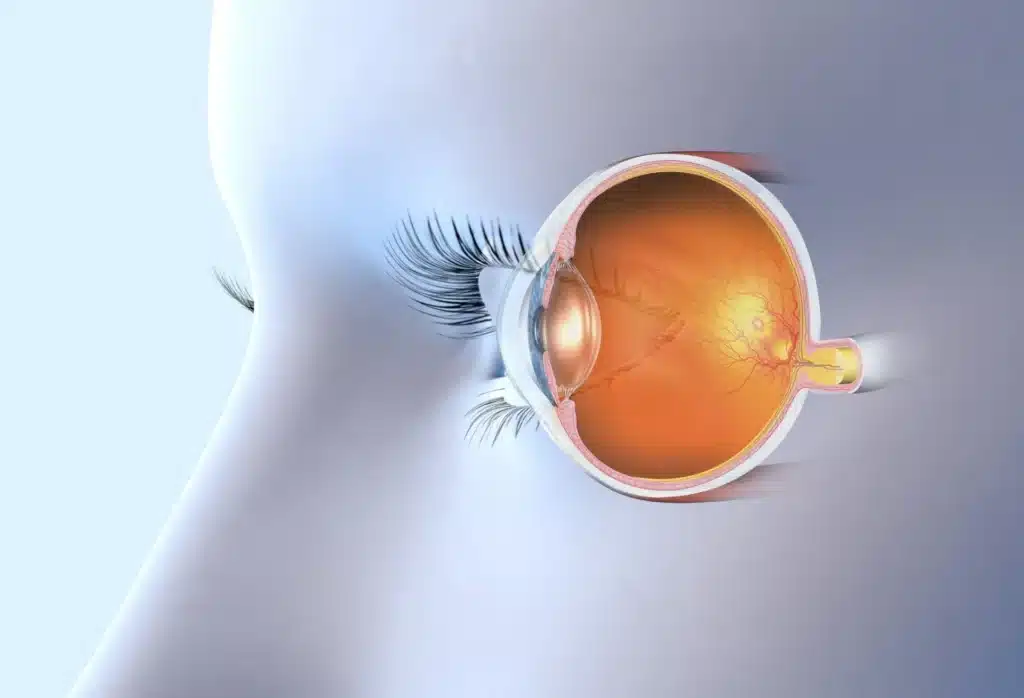
Of all the different structures that make up the eye, the macula is one of the most powerful and important. It’s located in the center of the retina, which is where light rays are refracted once they pass through the cornea and lens. From there, they travel to the brain via the optic nerve.
The macula might be just 5mm in diameter, but it plays a primary role in both eye health and function – including central vision, fine detail, and color perception. Once light rays hit the macula, it converts them into electrical signals, which are converted into an image by the brain.
Like any other structure in the eye, the macula is subject to a number of diseases and other issues that might cause damage – especially as we age. While this can cause vision loss or impairment, there are treatments available that can help prevent further damage to the macula.
What is Age-Related Macular Degeneration (AMD)?
Macular degeneration, also known as age-related macular degeneration (AMD), is an eye disease that’s characterized by damage to the macula – normally a result of the natural aging process. As the cells in the macula start to deteriorate, so does the function of the macula.
There are four primary stages to macular degeneration:
- Sub-Clinical AMD – this stage occurs before any physical or visible changes to the macula. One of the earliest and most common symptoms is poor night vision.
- Early AMD – although patients rarely experience vision loss and/or pigmentary abnormalities during the early stage, medium-sized drusen are present during an exam.
- Intermediate AMD – with intermediate macular degeneration, drusen are growing larger and patients usually experience blurred central vision, contrast sensitivity, and pigmentary abnormalities.
- Late AMD – also known as advanced macular degeneration, this stage is characterized by noticeable vision loss, either due to geographic atrophy or choroidal neovascularization.
Macular degeneration is the leading cause of severe vision loss in patients over the age of 65 – affecting more than 10 million (as many as 15 million) adults in the United States. That number is expected to nearly double over the next few decades, an alarming and unnerving statistic.
What Causes Macular Degeneration?
Researchers aren’t 100% certain what causes macular degeneration, but they believe genetics, heredity, aging, lifestyle choices, and environmental factors play a role in its development. In general, caucasians have an increased risk of developing AMD, as well as women over men.
With that said, there are two primary types of age-related macular degeneration – wet AMD and dry AMD. The causes and symptoms will differ depending on what type of macular degeneration you have, making the diagnosis essential to learning how to cope with and live with the disease.
Let’s take a closer look at the two types of AMD below:
Dry AMD
Dry AMD, also known as the atrophic type, is the most common form of macular degeneration – roughly 85-90% of all AMD patients have the dry form. It’s generally caused by tiny clumps of fat and protein, called drusen, that develop under the retina and in the macula, obstructing vision.
The symptoms of dry macular degeneration are almost non-existent in the early stages. Over time, the drusen grows larger and central vision (along with color perception) grows worse. As of right now, there are no cures or treatments for dry AMD, though there are ways to prevent it.
Wet AMD
Wet AMD, also known as exudative type, is a much more rare form of macular degeneration – roughly 10-15% of all AMD patients have the wet form. It’s generally characterized by abnormal blood vessels grow and leaking under the retina. As the vessels leak, they scar the macula.
Most people don’t know they have wet macular degeneration until it’s in the later stages, which is why it’s viewed as the more severe and dangerous form of AMD. Treatments do exist, but results may vary. Most people will preserve existing vision and/or slow the progression of AMD.
How Long Does it Take to Lose Vision With Macular Degeneration?
The rate of progression for macular degeneration depends on the type of AMD the patient is diagnosed with. On average, most patients see symptoms gradually worsen over the course of 5-10 years – though some forms of wet AMD develop within days of experiencing symptoms.
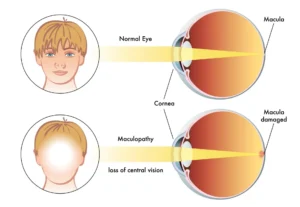
While patients can experience significant vision loss due to AMD, the disease will never cause full blindness.
This is because macular degeneration doesn’t affect an individual’s peripheral vision – just their central vision and color perception.
With that being said, macular degeneration can make it extremely difficult to read, recognize faces, drive, and notice fine details in your visual field. Symptoms include loss of central vision, distorted vision, wavy or curved lines, lack of color, and/or dark areas in your field of vision.
How to Prevent Macular Degeneration
While there are no treatments for dry AMD, there are ways to reduce your risk or prevent further damage to the macula. For example, patients are usually asked to exercise regularly, quit smoking tobacco, wear UV-protective glasses, control body weight, and control blood pressure.
Eye doctors also ask patients to follow a healthy diet – here’s a look at what foods should be eaten and what foods should be avoided with macular degeneration:
- Avoid: processed foods, foods rich in trans fats, tropical oils, margarine, vegetable shortening, high-fat dairy foods, fatty beef, lamb, pork
- Eat: frutis, vegetables, fish, nuts, seeds, Mediterranean-style diet, antioxidants, Omega-3 fatty acids, zinc, copper
- Supplements to Take: Vitamin C (500 mg), Vitamin E (400 IU), Lutein (10 mg), Zeaxanthin (2 mg), Zinc (80 mg), Copper (2 mg)
For those that are diagnosed with wet AMD, treatment might include the use of anti-VEGF drugs – which prevent blood vessels from forming in the retina. Blood vessels can also be removed via laser surgery to prevent or slow fluids leaking into the macula. Either way, there is hope.
Are you starting to experience symptoms of macular degeneration? Are you worried that your vision loss is a result of damage to the macula or retina? To schedule an appointment with a dedicated and experienced eye doctor, contact Milwaukee Eye Surgeons at (414) 377-5550.